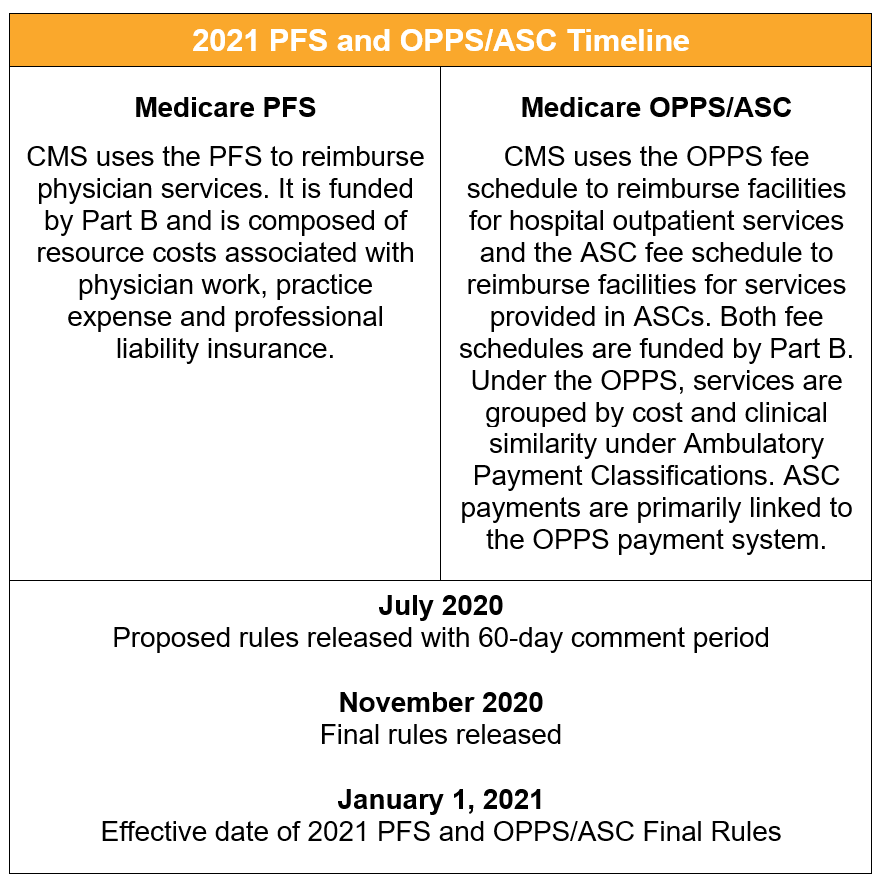
The Centers for Medicare and Medicaid Services (CMS) will soon release the 2021 Medicare Physician Fee Schedule (PFS) and the Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center (OPPS/ASC) Proposed Rules. These rules will have a significant impact on Medicare fee-for-service spending on physician and hospital outpatient services, and on quality reporting in calendar year (CY) 2021. Below we have detailed key issues to watch for in both rules.
The unexpected but undeniable shadow hanging over the 2021 payment rules is the Coronavirus (COVID-19) pandemic. The crisis has had a dramatic impact on the healthcare system, including Medicare physician and hospital outpatient services. Uncertainty regarding when and how the pandemic will end creates challenges for the strategic planning and decision making that is required of an annual rule like the PFS or OPPS/ASC.
Since the public health emergency (PHE) was declared earlier this year, the Trump Administration has issued waivers to reduce regulatory burden, and the US Congress has allocated funds to ease the financial stress on providers. The 2021 payment rules may clarify whether CMS will continue to seek to accommodate providers by how aggressively they propose to implement new policies and if they extend or make permanent temporary flexibilities implemented through COVID-19 waivers.
A key change implemented through COVID-19 waivers was expanded flexibility for telehealth services, which has led to an uptick in the use of telehealth, remote patient monitoring and communication-technology-based services. There is some expectation that CMS will address telehealth in the upcoming rules. In recent public comments, CMS senior leadership indicated that they will use the PFS proposed rule as a vehicle to propose making certain temporary telehealth waivers permanent. Another indication that CMS may address telehealth in these rules is CMS’s recent proposal in the CY 2021 Home Health Proposed Rule to make temporary COVID-19 telehealth flexibilities for home health services permanent.
How will CMS balance budget neutrality and increased payments for office/outpatient evaluation management (E/M) codes in CY 2021?
In the CY 2020 Final Rule, CMS finalized its proposal to adopt increased payment rates for office/outpatient E/M codes in CY 2021. While the precise impact is unknown until the CY 2021 PFS Proposed Rule is released, these payment changes will reallocate billions of dollars in the PFS. Since changes under the Medicare PFS are required to be budget neutral, to offset increased spending from the finalized E/M changes, CMS would need to implement corresponding fee reductions. These reductions would likely be implemented through a reduction in the physician conversion factor. The net impact will depend upon the mix of services performed by individual practices. For example, certain specialties that perform a high volume of E/M services (e.g. family physicians) may experience an overall positive impact, while others such as specialists who do not report E/M services in high volume, will generally experience an overall negative impact as a result of these payment changes.
Stakeholders have been advocating with both Congress and CMS to reduce the negative impact of these payment rate changes. Congress is able to allocate funding to address budget shortfalls or even suspend the application of budget neutrality—but even if Congress does act, it likely will not be until the end of the year. CMS has more limited options available and must indicate how it will implement this reallocation of spending in the CY 2021 PFS Proposed Rule. In light of the impact of COVID-19 on physician practices, some stakeholders have called on CMS to delay the implementation of these changes for one year. CMS also could choose to phase in the changes over a multi-year period. This option would slow down, but not reduce, the overall impact of the payment changes.
Will CMS continue to expand services such as remote care, care coordination and management, and opioid treatment services?
In recent years, CMS has expanded, increased payment and provided greater flexibility around remote care services and care coordination and management services. CMS has also responded to the opioid crisis by promoting evidence-based pain management protocols and providing ways for patients to access treatment for opioid use disorder. The CY 2020 PFS final rule included several new codes and increased payments for services in these areas. COVID-19 has brought increased interest in remote and telehealth services and unfortunately, the addiction treatment services community has raised concerns that the pandemic is a risk factor for opioid relapse. In light of increased attention to these issues, CMS could choose to propose additional codes or greater flexibilities for these services in the CY 2021 PFS Proposed Rule.
Will CMS fully implement the Appropriate Use Criteria (AUC) program in 2021?
The Protecting Access to Medicare Act of 2014, Section 218(b), established the AUC program. Under this program, a practitioner who orders an advanced diagnostic imaging service for a Medicare beneficiary would be required to consult and report measures through a qualified Clinical Decision Support Mechanism. The AUC program was originally scheduled to be implemented in 2020. CMS established the first year as an educational and operations testing period with no payment consequences. The program has been criticized as burdensome, duplicative of other programs and costly; furthermore questions have been raised on the overall effectiveness of the program. While CMS previously indicated that the program will be fully implemented on January 1, 2021, it remains to be seen whether CMS will allow some level of flexibilities for another year.
Expanding scope of practice for non-physician healthcare providers has been a priority for this Administration, even before the pandemic. Will CMS propose additional flexibilities?
In the CY 2020 PFS Final Rule, CMS relaxed supervision requirements for non-physician healthcare providers. Several COVID-19 waivers also expanded scope of practice, allowing non-physician clinicians to practice to the full scope of their licenses. CMS may continue this trend by proposing to make COVID-19 waivers related to flexibilities around scope of practice permanent or they could propose additional policies that allow non-physicians to practice at the top of their license.
CMS has already announced flexibilities for the 2020 Performance Year of the Merit-based Incentive Payment System (MIPS). Will CMS propose further flexibilities? Will the agency defer the previously finalized proposal to transition to the MIPS Value Pathway (MVP) framework in CY 2021?
MIPS-eligible clinicians have their payments increased, maintained or decreased based on relative performance in four quality-related, interoperability and cost performance categories. In the CY 2020 PFS Final Rule, CMS indicated that it will begin to transition MIPS to the MVP framework beginning in CY 2021. Under the MVP, clinicians will report on a unified set of measures and activities centered around a specific condition or specialty.
In June 2020, CMS announced that MIPS clinicians may opt-out completely or partially from the 2020 MIPS Performance Year by completing a hardship exemption application and indicating that the hardship is due to the COVID-19 PHE. CMS might announce further flexibilities or delay the transition to the MVP framework in the CY 2021 PFS Proposed Rule.
Will CMS expand the scope of its prior authorization program?
In the CY 2020 OPPS/ASC rulemaking, CMS finalized its proposal to establish a process through which hospitals must submit a prior authorization request for a provisional affirmation of coverage before a specified covered outpatient service is furnished to the beneficiary and before the claim is submitted for processing. This policy currently is limited to five services furnished in a hospital setting with an implementation date of July 1, 2020. It is unclear whether CMS will expand upon the scope of services for 2021 with no experience on the initial implementation by the time the proposed rule is released or hold off until 2022 for any changes to its policy.
Will CMS revise or expand upon its price transparency policies?
For CY 2020, CMS finalized its policy requiring hospitals to establish, update and make public a list of their standard charges for the items and services they provide, including negotiated prices with third-party payors. While several stakeholders filed suit challenging the legality of this rule, the district court sided with CMS and upheld the hospital price transparency rule. Pending an appeal, hospitals are preparing for the rule’s January 1, 2021, implementation date. In light of stakeholder’s concerns about the rule and the pressures of the COVID-19 public health emergency, it is uncertain whether CMS will make any revisions to the policy as originally proposed/finalized.
Will CMS make any changes to its site neutrality policies?
In 2019, as a continuation of its site neutrality policies, CMS implemented a policy that reduced OPPS payments for clinic visits described by HCPCS code G0463 and furnished by off-campus provider-based outpatient departments that previously were excepted or grandfathered from site-neutral payment policies. This policy was phased in over a two-year period, with the second portion of the payment reduction occurring in 2020. Given ongoing litigation and a 2019 ruling against CMS (citing lack of statutory authority) together with the pressures due to COVID-19, it is unclear what actions CMS might take regarding its site neutrality policies in the proposed rule.
Will CMS expand upon the list of services permitted in the hospital outpatient and ASC setting?
In the CY 2020 rulemaking cycle, CMS removed several procedures from the inpatient-only list and expanded the covered procedures list in the ASC setting. In light of the other policy changes and the COVID-19 PHE, CMS may seek to expand the list of services to be performed in the outpatient setting.
Other issues to monitor for possible action include:
The CY 2021 PFS and OPPS/ASC Proposed Rules are scheduled to be released in July 2020. After the rules are released, McDermottPlus will host a webinar to analyze the major proposals. When available, registration information will be available on our website.
Please visit our resource centers for more information:
For more information contact Deborah Godes or Sheila Madhani.