McDermottPlus is pleased to bring you Regs & Eggs, a weekly Regulatory Affairs blog by Jeffrey Davis. Click here to subscribe to future blog posts.
April 18, 2024 – Last week, the Centers for Medicare & Medicaid Services (CMS) released the Fiscal Year 2025 Inpatient Prospective Payment System (IPPS) proposed regulation. This 1,900+ page annual reg updates Medicare payments and policies for hospitals and long-term care hospitals – and it includes a plethora of major proposals that affect hospitals, clinicians and patients. Our full summary of the reg can be found here.
Embedded within this massive reg is a proposal from the Center for Medicare and Medicaid Innovation (CMMI) within CMS to initiate a new episode-based payment model that hospitals in certain geographic areas would be required to participate in starting in 2026. To help me dig into the proposed Transforming Episode Accountability Model (TEAM), I’m bringing in my colleague Kristen O’Brien.
Before discussing the TEAM proposal itself, it is important to understand its context. CMMI has implemented more than 50 models that are meant to test alternative approaches to paying for care in both Medicare and Medicaid. The vast majority of these payment models are voluntary, meaning that providers do not have to participate. CMMI argues that voluntary models lead to “selection bias,” where providers who know that they will do well in the model actually participate – leading to less overall savings to the Medicare program and a poorer evaluation, thereby decreasing the chance that the model could be successful if expanded or made permanent. On the other hand, mandatory models, in CMMI’s view, have a better chance of achieving results that could be scalable. Despite touting the benefits of mandatory versus voluntary models, the Biden Administration has not implemented any CMMI models that would require certain providers to participate (until now). Unlike voluntary models, mandatory models must go through notice-and-comment rulemaking to be established.
TEAM didn’t come out of thin air. Last July, CMMI released a request for information on a possible mandatory episode-based payment model based on its experience testing similar models, including Bundled Payments for Care Improvement, Bundled Payments for Care Improvement Advanced and the Comprehensive Care for Joint Replacement (CJR) model. A stand-alone reg related to a new episode-based payment model was also found in the Biden Administration’s fall 2023 unified agenda, which announces upcoming regs.
What was surprising (at least to us) was that CMMI proposed the new payment model in the IPPS reg. Proposing a mandatory model (again, the first mandatory model in the Biden Administration) is monumental, and it could have warranted its own separate reg. CMMI describes each facet of the model in significant detail in the IPPS rule and seeks comment on every element. In order for the model to actually be implemented, CMMI must finalize the model in the FY 2025 IPPS final reg or another final reg.
While we will not go over every detail of TEAM, here are some core proposed features of the model:
CMMI proposes that the model will last for five years from January 1, 2026, to December 31, 2030. This means the model may not start under the current Administration and could hinge on new leadership at CMMI. Further, starting in 2026 coincides with the intended end date of similar bundled payment models (e.g., the CJR model is set to expire in 2024).
Acute hospitals that are paid under the IPPS and initiate episodes in selected geographic regions would be required to participate. Some hospitals aren’t paid under the IPPS and therefore would be excluded. For example, since hospitals in Maryland have their own special payment rules and are not paid under the IPPS, all acute care hospitals in Maryland would be excluded. Participant hospitals can enter into sharing arrangements with other providers. In other words, in order to be successful in the model, hospitals can get buy-in from other providers and agree to share any reconciliation payments (described below) with the providers. On a separate but related note, TEAM participants may also choose to provide in-kind patient engagement incentives to beneficiaries in an episode.
CMMI considered proposing that participation in TEAM be voluntary but was concerned that a fully voluntary model would not lead to meaningful evaluation findings. CMMI seeks comment on allowing hospitals that have previously participated (or are currently participating) in a Medicare episode-based payment model and that are not in a selected geographic region to voluntarily opt in to TEAM.
CMMI proposes to choose acute care hospitals for participation based on inclusion in core-based statistical areas (CBSAs) and to use a stratified random sampling method to select approximately 25% of eligible CBSAs (ineligible CBSAs include those in Maryland and CBSAs in which no episodes were initiated at hospitals for any of the five episode categories discussed below). CMMI states that there are 803 eligible CBSAs, so about 200 would be selected for the model.
CMMI would first stratify CBSAs into groups based on average historical episode spending, the number of hospitals, the number of safety net hospitals and the CBSA’s exposure to prior CMMI bundled payment models. Then CMMI would randomly select CBSAs from each category, oversampling CBSAs with certain characteristics.
CMMI proposes to test five surgical episodes in the model: Coronary Artery Bypass Grafting, Lower Extremity Joint Replacement (LEJR), surgical Hip and Femur Fracture Treatment, Spinal Fusion and Major Bowel Procedure. All items and services paid under Medicare Part A and Part B (including most Part B drugs with specific exclusions) would be included in the episode. The episode would begin with an “anchor” acute care hospital stay or hospital outpatient department procedure visit and continue 30 days after discharge from the anchor hospitalization or anchor procedure.
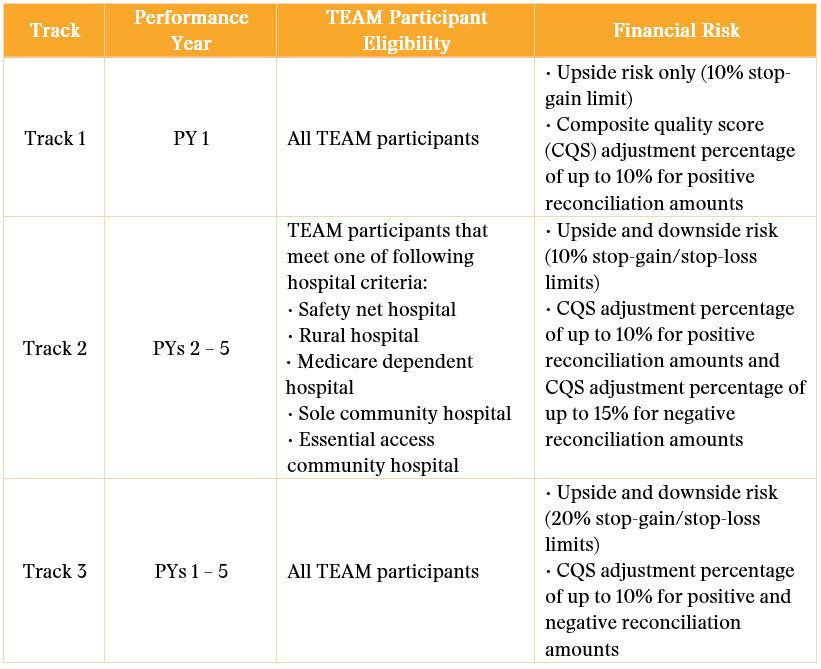
CMMI proposes that the TEAM participant (the hospital) would be fully financially responsible for the episode (again, the hospital can enter into financial arrangements with other providers). CMMI would offer three participation tracks to provide a glide path to risk:
As seen in the chart below, Track 3 has the highest potential for savings (and losses), with a maximum upside and downside of 20% of the target price (called the stop-gain/stop-loss).
CMMI proposes specific quality measures for TEAM, all of which can be reported through the Hospital Inpatient Quality Reporting Program.
A participant’s performance on these measures would impact the size of the positive or negative reconciliation amount the participant would be eligible to receive.
CMMI proposes to use three years of baseline data, trended forward to the performance year, to calculate target prices at the level of MS-DRG/HCPCS episode type and region. CMMI would risk-adjust episode-level target prices. This approach would be consistent with PYs 4 – 8 of CJR. CMMI proposes to apply a 3% discount factor to the benchmark price to serve as Medicare’s portion of reduced expenditures from the episode.
CMMI proposes to conduct an annual reconciliation in which CMMI would compare spending for a TEAM participant’s beneficiaries in episodes against the reconciliation target price to determine if CMMI owes the TEAM participant a reconciliation payment, or if the TEAM participant owes CMMI a repayment (for all Track 3 participants and beginning in PY 2 for Track 2 hospitals). CMMI would conduct the annual reconciliation of each TEAM participant’s actual episode payments against the target price(s) six months after the end of the PY.
Finally, CMMI proposes an appeal process for TEAM participants to contest matters related to payment or reconciliation.
CMMI proposes that TEAM participants would be required to screen attributed TEAM beneficiaries for societal risk factors such as food insecurity, housing instability, transportation needs and utilities difficulty.
CMMI proposes specific waivers under its innovation center authority (Section 1115A of the Social Security Act) similar to the waivers granted to existing episode-based payment models.
CMMI does not proposing to waive the homebound requirement under TEAM, but it does propose waiving the geographic and originating site Medicare telehealth requirements (currently waived through the end of 2024) and the requirement that Medicare beneficiaries have a prior inpatient hospital stay of no fewer than three consecutive days to be eligible for coverage of inpatient skilled nursing facility care.
CMMI also proposes other features of the model related to:
Public comments on this extensive model proposal and the rest of the FY 2025 IPPS proposed reg are due on June 10, 2024. By law, CMS must finalize the FY 2025 IPPS final reg by August 1, 2024 (60 days prior to the start of the fiscal year on October 1, 2024). We believe that this model will garner a lot of comments, and it will be interesting to see whether CMMI has time to work through them all prior to August 1. If CMMI can’t do so, then it may finalize the model in a separate final reg released later in the year.
Until next week, this is Jeffrey (and Kristen) saying, enjoy reading regs with your eggs.
For more information, please contact Jeffrey Davis. To subscribe to Regs & Eggs, please CLICK HERE.